BPA5599 - SECTION 3: MEDICAL - MENTAL HEALTH DIFFERENTIAL DIAGNOSIS

Section 3: Medical - Mental Health Differential Diagnosis
Physicians who are general practitioners have at their disposal numerous articles and guidelines to help heighten their awareness of mental health symptoms and diagnoses - even when their patients identify their problems as medical complaints. In this regard, generalists have a broader based perspective where patients seek help for physical complaints when the true problem is psychological or emotional in nature, or vice versa.
Mental health clinicians are well advised to keep their own reminders in this area. If mental health clinicians encounter deepening signs of depressive illness, a diagnosis made too quickly or too facilely may miss potential physical causes for the depression. A good biopsychosocial assessment should be entered into with flexible thinking and a broad-ranging search for the primary cause or etiology of the client's problems - including awareness of the possibility that a medical reason for the presenting problems may be the better explanation.
In the 21st Century, with a healthcare system that is less than ideal, it is not unusual for a mental health clinician to be the first point of contact for a client seeking care to address an increase in anxiety or depression. The client may enter into the healthcare system through an Employee Assistance Program, or may simply seek out the services of a mental health clinician because the presenting problems appears to be psychological in nature.
However, depressive symptoms are often the initial symptoms of some physical diseases, the aftermath of trauma, or side effects from prescribed medications. When the medical illness goes untreated, psychiatric treatment only addresses the symptoms – leaving untreated potentially severe and life-threatening medical problems.
For instance, research has found that biologic relationships exist between malignancies (cancers) and depressive syndromes. Depressive symptoms are associated with cancer in up to 50% of cases. On many occasions the onset of depression is the first indication of undetected carcinoma (cancer). The depressions exhibited by the patient range from adjustment disorder with depressed mood to major depression.
The responsibility for the mental health clinician here lies in conducting a thorough enough assessment to direct the patient to the medical resources that will best target the real problems. Whereas all physicians receive at least a rudimentary introduction to mental health problems, most mental health clinicians are largely untrained and unskilled in looking for the signs and symptoms that could be indicative of underlying physical illnesses.
There are numerous examples of lifesaving referrals from mental health professionals to medical specialists. Some particularly powerful examples were:
- A severely depressed woman admitted to a psychiatric unit in a medical hospital for severe headaches that her primary care physician ruled to be psychosomatic. Fortunately, the team quickly sought another opinion and her malignant brain tumor was treated surgically with success.
- A successful differential medical diagnosis of an older depressed gentleman who had decreased appetite and fatigue, which turned out to be the result of stomach cancer.
- A Nurse Clinical Specialist in Psych/Mental Health cautioned a friend to seek medical help rather than an antidepressant for the hopelessness she was feeling in her pain management treatment. Her back pain had persisted and she had a cracked rib. As the nurse suspected, her diagnosis was Multiple Myeloma, a malignant cancer of the plasma cells and bone marrow which ultimately took her life.
In some cases, the depressive symptoms are caused by the frustration, discomfort and hopelessness these patients experience secondary to their physical symptoms. However, there are brain-body connections that may cause clients to have a deep below-consciousness awareness of some change to their overall homeostasis from the presence of the medical problem. It is the role of all healthcare professionals to be cognizant of such possibilities, and to make referrals whenever appropriate.
What often prevents adequate diagnosis from either medical or mental health practitioners is incomplete information from insufficiently conscientious assessment processes. Depression - and medical or other psychiatric illnesses - may be linked biologically, psychologically - or may appear to be entirely unrelated. For this reason, a thorough assessment is one that considers the presence of physical illness or other physiological factors, in addition to the presence of a mental or emotional disorder.
Roles and Boundaries for the Mental Health Clinician
The role of the mental health clinician in determining the presence of medical conditions as part of the biopsychosocial assessment is limited by licensure guidelines. It is not the place of a mental health clinician to arrive at a medical diagnosis for any client who presents, even it all of the evidence points in the direction of a medical cause that the clinician has seen many times in the course of his/her practice - and/or has experienced him/herself.
Legally and ethically, there is a clear boundary that must be observed concerning what falls within the area of competence of the clinician. The role of the mental health clinician lies in making an appropriate referral of the client to medical personnel qualified to continue the biological components of the case formulation, arrive at an appropriate diagnosis, and formulate the proper treatment plan.
But clinicians must also not stay within their own narrow lane. They must retain some awareness of the many ways in which medical problems may create mental health symptoms, and have enough knowledge of what to look for that they can make a compelling case to the client for seeking out additional medical care. It is possible to serve as a consultant to the client without stepping over the boundary line into areas that exceed your licensure.
Below are two ways to have that conversation. The first way would represent a boundary violation and put the clinician at risk for ethical challenges. The second way would remain within the proper boundary lines, but would still create motivation for the client to seek out appropriate medical care.
Wrong way:
"I am seeing signs and symptoms of some kind of thyroid condition that may be making you alternate between periods of excessive energy and extreme fatigue. I think you should consider seeking out someone who could get you on Synthroid or Levithroid."
Better way:
"I am seeing some things that suggest a need for some additional help to figure out what is going on. It may be that you are having a mental health problem that is causing you to have these mood swings, but there are also some medical conditions that I would like have ruled out before we continue with our work. I'd like to have you speak with your primary care physician about these signs and symptoms to see if he/she thinks some further testing might be indicated. If there aren't any medical things happening, it helps us know what we are dealing with. But if there are medical causes for this, then we need to know this, and then there may be some medications that will make your situation improve pretty quickly, and may preclude the need for counseling. As a mental health clinician, I'm not the right person to make a determination about any medical causes for your symptoms. But I do have enough experience and training to know when it is time for a referral and how important it might be for you to get the right kind of help if it is needed. Can I count on you following through on discussing this with your doctor?"
The Knowledge Base Mental Health Clinicians Should Have in this Area
As you read the material in this chapter, consider how the information presented may provide a greater understanding of when to consider a referral to a qualified medical provider for further diagnostic assessment.
Depression/Anxiety Caused by or Indicating Medical Illness
Some medical situations lead directly to brain cell (neuron) destruction with resulting mental impairment and mood changes. Appropriate intervention depends on the ability to recognize changes in mental status that may be due to brain tissue injury, as well as to disorders of mood and thought.
Neurologic destruction--brain cell and tissue damage--can come from direct or indirect sources: Accordingly, mental health clinicians should include in their biopsychosocial assessment questions about a history of experiences that may have led to brain injuries: accidents, illnesses with high fevers, strokes or heart attacks, domestic violence or physical fights, or contact sports such as football or soccer where there may be cumulative brain damage over a number of years.
Direct brain cell and tissue damage:
- Brain trauma
- Ischemia (cellular breakdown)
- Infarction (cerebral-vascular accident, or stroke)
- Abnormal neuron growth (tumor)
- Degenerative brain cell loss
Indirect brain cell and tissue damage:
- Dysfunctions of brain metabolism associated with diseases that poison the whole system
- Body trauma
DIRECT BRAIN CELL AND TISSUE DAMAGE
Brain Trauma
Brain trauma can be responsible for depression or anxiety for a number of reasons.
There may be temporary or permanent injury to parts of the brain that are responsible for personality and mood. Millions of people have significant head trauma every year in the United States. Trauma takes three forms:
- Blunt trauma – such as occurs in falls or blows to the head. These can occur as violently as in a car accident or as innocently as on a soccer field when using the head to pass the ball.
- Penetrating head wounds – occurring from such external objects as bullets, spikes or other sharp foreign objects that enter the brain and cause localized destruction.
- Indirect trauma – such as blast injuries or whiplash movements of the neck. The trauma to the brain may not be localized at any one point of injury. (30)
In all cases the damaging forces are having their effects on a relatively moveable brain limited by a fixed skull, dura mater (fibrous covering of the brain), cranial nerves, blood vessels and brain stem. In much the same way as when gelatin shakes within a closed container, brain tissue movement against the intracranial cavity can cause random bruising and inflammation.
Penetrating head wounds directly damage tissue, but also send shock waves through the brain causing tissue destruction some distance from the path of the penetrating object. This process will be detailed further in the section on body trauma.
After the initial injury and after apparent recovery there may remain symptoms of irritability, short attention span and emotional lability. Stressful situations may become unmanageable. However, the primary psychological manifestation of brain injury is depression.
A thorough assessment process should always include the gathering of information about potential head trauma. It should examine not only the routine ways in which a head trauma may occur, but also hidden or unusual ways. For instance, recent studies have shown some potentially troubling correlations between youth soccer – where soccer balls are repeatedly “headed” by the players – and brain trauma.
The implications of this are important. The client may not always be aware that he/she has experienced a trauma serious enough to cause concern. In the movies, the hero is often knocked unconscious with a blunt object to the back of the head. Soon thereafter, he or she wakes up, shakes off the injury and proceeds to save the world.
In reality, a relatively small amount of trauma can produce some fairly dramatic and sometimes durable consequences. The client who takes his or her cues from the movie version of a head injury can erroneously assume that there is little cause for concern. The clinician who conducts a thorough assessment of a client should not be quite so cavalier concerning this potential difficulty.
A discussion of physical activities and injuries should always be included in a thorough assessment to rule out brain trauma as a cause for depression and anxiety. Subtle changes in behavior, mood, drive, information processing - as well as motor control and spatial relationship skills - may be affected where brain trauma is suspected.
The specific effects of the head injury depend on the location and severity of the initial injury. As noted in the discussion of brain physiology and anatomy, different areas of the brain have their own functions, and their interactions with each other are critical to normal physical and emotional functioning. Note the diagram below that shows areas of the cerebral cortex as affected by tissue destruction.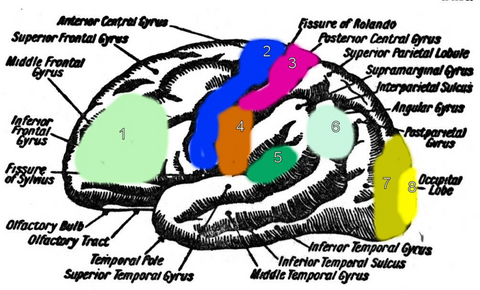
Area 1 (Light green) Frontal and pre-frontal cortex. Brain injury here causes changes in mentation: Memory, personality, affect, motivation, judgment, reasoning problems
Area 2 (Blue) Motor cortex. Brain injury here causes motor disability: left side problems for injury on the right motor cortex, right side problems for injury on the left motor cortex
Area 3 (Pink) Sensory cortex. Brain injury here causes damage to the ability to receive sensory inputs
Area 4 (Orange) Speech area. Brain injury here causes expressive aphasia (inability to speak)
Area 5 (Dark green) Speech area. Brain injury here causes receptive aphasia (inability to understand speech and language)
Area 6 (Light blue-green) Auditory and speech area. Brain injury here causes a variety of auditory and speech problems.
Area 7 (Dark yellow) Visual cortex. Brain injury here causes visual loss
Area 8 (Bright yellow) Visual cortex. Brain injury here causes cortical blindness
Ischemia and Infarction
Injury to the brain can cause direct cell destruction - as previously discussed in our section on head trauma - or can cause a domino-effect of cell breakdown called ischemia. This process begins with hypoxia (lack of oxygen to the cells). The loss of oxygen can be the result of a number of factors related to trauma, injury or disease.
Hypoxia is followed by a failure of ion exchange across the cell membrane. This means that chemicals important to healthy brain functioning – like potassium - are not able to operate in a manner necessary to maintain healthy neuron functioning. The result can be edema (swelling from body fluids) with its influx of calcium ions, free-radical production, and lipid peroxidation (fat metabolism), which can ultimately lead to complete cell destruction and severely alter neurotransmitter functioning. (8)
However, there may also be changes in the metabolism of certain enzymes after brain cell death, such that ischemia may lead to mood disturbances and cognitive dysfunction. The severity of the injury, related to the duration and degree of ischemia, as well as the location of the injury, determine the long term effects on the individual. Complete ischemia is the cause of brain infarction known as cerebral-vascular accident, more commonly known as a stroke.
For normal brain functioning, to occur, certain neurotransmitter pathways must be functioning properly. Dopamine is necessary for the transmission of motor messages, managing of the appropriate level of anxiety, mood, and motivation. Epinephrine supports learning and memory. Serotonin affects alertness, the overall sense of well-being, and information processing.
With brain cell injury, these pathways may be temporarily impaired due to the immediate injury, or due to swelling or compression that follows the injury. If the injury is severe enough, the pathways may be permanently blocked or may function only marginally. (8) Depression is due to the alterations that are created in the biochemical neurotransmitter systems.
There are several factors affecting the likelihood and severity of depression. These should all be assessed, and they include:
- Location of the lesion
- Family history of depression
- Pre-morbid depression history
- Pre-stroke social functioning
Abnormal Neuron Growth/Tumor
Tumor activity may lead to brain cell destruction in a variety of ways. The first is through the overproduction of mutant cells that replace functioning cells, leaving areas of impaired neuronal transmission. Likewise, the proliferation of tumor cells may take up space and compress the healthy brain tissue, leading to ischemia. Dangerous byproducts of cancer cell metabolism may also lead to neuronal toxicity and cause destruction of brain tissue. (22)
Brain tumor activity can present itself as sudden changes in mood, often with anger and agitation. Manifestations of the illness are dependent on the areas of the brain affected by the tumor activity. We have already discussed some of the effects in our earlier section on brain physiology.
It may also be helpful to mention pheochromocytoma, a tumor of the adrenal medulla. This ailment produces severe hypertension and anxiety attacks by causing the adrenal glands to produce excess adrenaline. The DSM-5 lists this as one of the most likely endocrinological ailments to produce anxiety states.
Uncovering these kinds of potential problems can be somewhat complicated. Often, a client's changed mood will result in different behaviors towards others, specifically increased agitation or aggression. This may in turn cause changes in the behaviors and mood of others with whom they interact. Other people may withdraw from or get angry at the client. The client's lack of insight may preclude awareness of changes in his or her own mood and behaviors. He or she may instead blame their increasing problems on others.
When the changes in behaviors and mood occur more rapidly, through head injury, sudden illness, or the presence of neurotoxic chemicals that destroy brain tissue, it is often easier to note the change in behavior and mood. A slow growing tumor, on the other hand, can slowly shift mood and behavior, making it more difficult to identify a medical process as the precipitant.
Degenerative Brain Cell Loss
Brain cell loss can be caused directly through degenerative illnesses such as Parkinson’s disease and Alzheimer’s. Depending on the area of the brain that is affected, the first symptom may be depression. Alzheimer’s patients and those with dementia have decreased intellectual functioning that also leads to depression. Depression in this population is as high as 60%. (9)
There is a neuronal degeneration in these diseases. Neuro-chemical changes –including the loss of dopamine secretion and a decrease in dopamine receptor sites in the neuronal pathways - contribute to the manifestations of mood disorders in these patients.
Depressed mood is also affected by the degree of functional impairment, how the individual is able to function in activities of daily living (ADL). Loss of the ability to communicate and to be responsible for self-care seem to be the highest indicators of mood disorders that can complicate rehabilitation, affect compliance and impact the overall healing of the body itself. (8)
At the other end of the age scale, it is also important to know that the Streptococcus Pneumoniae bacteria, a common source of ear infections (otitis media) in children, can lead to brain damage and cell loss in children's developing brains. (13, 18) Therefore, when conducting mental health examinations with children, it is important to gather any history of problems with repetitive ear infections or ear infections that went untreated for extended periods of time.
As mentioned previously, a thorough assessment will also look for any history of encephalitis or meningitis, since these serious brain infections can lead to brain tissue damage and loss.
INDIRECT BRAIN CELL AND TISSUE DAMAGE
Dysfunctions of Brain Metabolism Associated with Diseases and Disorders that Affect the Whole System
As noted, any process that causes disruption of brain chemistry can lead to brain cell loss and psychiatric symptoms. Diseases that attack the nervous system directly - such as multiple sclerosis (MS) - do their damage by affecting the metabolism within the cells. Symptoms depend on the areas affected and the extent of the damage. Depression is often one of the first symptoms in MS (8), occurring in 50% of MS cases. (9)
When dealing with a client with anger problems it is important to know that certain physical illnesses have an affect on brain chemistry and aggression. For instance, violence brought on by hypoglycemic episodes is the experience of many alcoholics regardless of whether or not they are drinking. (24)
Anthropological studies done in the 1970’s among the Quolla Indians of Central America shed light on the effects of hypoglycemic episodes. The Quollas have been known for centuries to have high rates of violence with murder common among them. Their diets were very poor: high in refined sugars and alcohol and short of basic nutrition. Every tribesman tested was hypoglycemic. Moreover, the most violent among them had supernormal surges of adrenaline when their glucose levels fell too low. (24)
This can explain the anger reactions in persons with hypoglycemia due to illness or poor diet but can easily transfer an understanding to the alcoholic who after an evening of drinking becomes abusive. There is a hypoglycemic state brought on by an evening of heavy drinking - and the adrenaline hits the bloodstream about the time the individual arrives home from a favorite bar. By the time the adrenaline is released, the reasoning brain (cerebral cortex) has been turned off or dulled leaving the animal brain in charge. In this is a recipe for danger from violent episodes, with the potential raised for verbal abuse or even physical aggression that can have tragic results.
Furthermore, if hypoglycemic alcoholics stop drinking but continue to consume large amounts of caffeine and refined sugars, the outbursts of irritability and sudden anger will continue. These symptoms disappear, however, when brain glucose levels are stabilized. (24)
The following physical conditions lower the threshold for triggering anger:
- Over-tiredness
- Hunger
- Sexual frustration
- Hormonal changes due to puberty, pre-menstruation, pregnancy, child birth and menopause
- Physical craving for addictive substances such as alcohol, nicotine, caffeine or other drugs
- Intoxication
- Physical injury
- Living with chronic or acute pain
- Hypoglycemia
- Medication effects
- Dementia
Cellular health within the body is dependent on a critical balance of nutrients entering and being used by the cells and of adequate mechanisms for the transfer of toxins out of the system. Many diseases that affect the body lead to high toxicity and/or poor elimination of toxins.
There are also disorders, such as Phenylketonuria (PKU), that can create toxic conditions in the brain through failures of the body to process certain essential amino acids or other substances necessary for metabolic or neurochemical functioning. The most common of these kinds of disorders is Diabetes Mellitus, which can cause depression due to the dysfunction of metabolism critical for brain activity.
Even basic nutritional deficits can show up as mental health symptoms. The neurotransmitters depend on a delicate balance of nutrition to produce the enzymes necessary for the pathways to be able to function. Deficiencies in vitamins and minerals can lead to brain chemical imbalances expressed as behavior problems, learning difficulties, dyslexia, mood disorders and insomnia. (47)
Vitamins and minerals are vital for behavior and brain function. A study of prisoners in England found that neurotransmitter imbalances may have been set up at an early age as a result of dietary choices.
They found that the high refined carbohydrate, high saturated fat diets that the prisoners chose were poor in vitamins and minerals, added to which the chemicals in colas and canned drinks disturbed the delicate brain function and interfered with the absorption of nutrients. They believe that some people are particularly sensitive to these types of chemicals, making them over-reactive and potentially violent. (22)
These researchers suggested a national policy of education on the benefits of healthy eating habits with vitamin and mineral rich fresh fruit and vegetables, brain oil rich oily fish, nuts and seeds to help prevent crime and poor behavior. (22)
Over time, individuals with diseases that lead to poor nutrient intake compromise their cellular functioning. Necessary elements for cellular regeneration are depleted and cells in the brain, as well as elsewhere, lose their ability to function. The diseases themselves may alter the body's ability to intake certain minerals or vitamins, or they may so affect appetite that important nutrients are left out of the diet.
For example, vitamin B6 is essential for the synthesis of neurotransmitters serotonin and dopamine. (40) A diet deficient in this vitamin - as can happen with excessive alcohol intake and poor overall nutrition - can lead to problems with neurotransmitter formation. Symptoms may appear that look like mental health problems.
There may also be occasions where problems occur related to excessive intake of certain vitamins and minerals. For instance, vitamin B6, in excessive doses, can result in nerve damage in the arms and legs. (40) Excessive amount of folic acid can lead to convulsions in people with epilepsy. (44) Manganese toxicity, usually found only in manganese miners, produces symptoms that resemble schizophrenia, with hallucinations and extreme irritability and increase potential for violence. (46)
Additionally, there are a variety of different genetic conditions whose effects involve the inability to absorb specific essential vitamins and minerals. Wilson's disease - a condition in which copper accumulates in the body and brain – is one such problem. The inability to transport copper across cell membranes results in toxicity and damage to the kidney and nervous system. (46)
Some of these genetic conditions are apparent at birth, while others manifest themselves later in life. Most of these problems can be identified with routine blood work if the client can be persuaded to seek health care and have a thorough physical exam.
It is always advisable to see what vitamin supplements clients are taking - or are not taking - in order to maintain good nutritional balance. It is also important to look for pronounced changes in appetite, taste, and overall nutritional health. Less well informed clients may be creating their own mental health problems with what they are putting in their bodies or withholding from their bodies.
Finally, recent advances in the treatment of autism suggest that some allergens may directly affect the brain tissue. Even such seemingly mild conditions as food intolerances, including gluten intolerance, lactose intolerance and other food and digestive ailments, may be the cause of psychiatric symptoms, including fatigue and malaise. (1)
Lactose intolerance is very common in certain populations, especially African, African-American and Asian populations. (41) Wheat intolerance, or celiac disease, is also not uncommon, particularly in people of European descent. (39) There appear to be genetic predispositions for many of these food related problems, and a history should probably include family history of problems with certain food groups.
These kinds of digestive difficulties will usually produce some physical manifestations, including headaches, nausea, weight loss and flatulence, in addition to the possible presence of such mental health concerns as lassitude or depression.
When performing a thorough assessment, it is helpful for the clinician to explore with the client what other physical symptoms might be present, so it can be determined whether there may be a medical problem at the root of the depression and lassitude. Referral should be made to a gastro-intestinal specialist for further examination when a physical problem is suspected.
In conclusion, while more research is necessary, the mental health professional should be aware of the possible effects of food intolerances and poor nutrition on the well being of their clients.
Statistic: The average length of time it takes for a symptomatic person to be diagnosed with Celiac Disease in the United States is eleven years.
Source: Characteristics of adult celiac disease in the USA: Results of a national survey, Green, PH et al., American Journal of Gastroenterology, 2001
Body Trauma
Because mental health clinicians typically have at least a beginning knowledge of the brain and neurological functioning, they are prepared to ask questions about a history of injury or illness that directly affects the brain. However, they are less likely to consider neurological effects of injuries and illnesses that occur in other parts of their clients' bodies.
Usually the neurotransmitters that are responsible for the responses of fear and anxiety are in balance and therefore primed to respond to threats in the environment. When a threat is perceived, information from the thalamus and cerebral cortex of the brain activates the hypothalamic-pituitary-adrenal (HPA) axis through their connection with the amygdala. Adrenal steroids are released and trigger the stress response in the body. (8)
Furthermore, most kinds of serious body trauma are perceived by the primitive systems of the brain as a threat. The chemistry of stress is triggered, and changes to a client's emotional state can be expected.
A complex neuro-chemical process ensues in which norepinephrine, y-aminobutyric acid (GABA) and serotonin are overwhelmed by the release of catecholamine. For instance, under the normal stress response, the norepinephrine receptors are balanced by the catecholamine receptors. (8)
In extreme stress due to trauma, the catecholamine is depleted by hyper-stimulation of the norepinephrine sites. This leaves the body system responding to increases of norepinephrine (adrenalin) with no buffer or balancing factors. This alters the cognitive and affective functioning of the individual, leading to symptoms similar to those of anxiety.
Persistent and severe stress can lead to a complete malfunction of the HPA axis and the secretion of high levels of catecholamines. Over time, these can be destructive to the physical systems of the body. Certain cancers, infections, myocardial disease (heart disease), and neurologic degenerative disorders are linked to chronic stress responses in individuals with poor adaptation skills for coping with trauma. (8)
The responses of every individual can be very different to pain – that is, how high a pain threshold they have and how much pain they can tolerate without severe emotional distress. These differences influence the degree of impact that pain will produce on the hypothalmic-pituitary-adrenal axis, whether the pain comes from body traumas or emotional traumas. Low pain tolerance creates more destruction through continuous imbalance at the catecholamine receptors.
CASE PRESENTATION
Your author encountered the effects of frontal lobe injury early in her career as a therapist. The prefrontal cortex is the region of the frontal lobe in the cerebral cortex behind the eyes which serves the “executive function” of integrating information and inhibiting emotional impulses that arise from the deeper brain centers like the limbic system. (31)
John had been a likeable, pleasant, hard working mechanic prior to a motorcycle accident that caused permanent damage to his frontal lobe. Since this is the area that helps to modulate primitive and spontaneous impulses, John’s behavior became socially maladaptive. He was spontaneously speaking whatever came to his mind - without filtering for appropriateness. He would swear, make sexually explicit comments, and become agitated easily. Finally, he acted out violently without the availability of higher level checks and balances on his impulses.
John was imprisoned for his behavior, but there was enough of the original functioning remaining for him to realize that he was unable to control his impulses. He became depressed and hopeless. Treatment options were limited because even if serotonin or other neurotransmitters were ingested, the physical pathways to transport these chemicals in his brain were no longer available. The cortical tissue was absent, so that he had no watchdog on the impulses arising from his limbic system. The damage was so severe that there was no tissue regeneration expected to occur.
As much of his higher executive functioning was lost, treatment focused on reducing the input of sensory information that he received through the internal stress receptors in his vital organs. He was given Inderal, a blood pressure medicine that acts on the autonomic nervous system.
The learner can appreciate the theory behind this treatment by recalling a time when you personally felt stress, a time when you actually felt the stress in your physical body before your conscious mind registered the thoughts of being stressed. One might experience a tightening in the “gut” or become aware of clenched fists. Imagine what it might be like to have all automatic, physical stress responses go directly to the brain’s emotional center for interpretation as “attack.”
In a stressful situation, the peripheral nervous system that functions with the internal organs and extremities sends messages via the autonomic nervous system and adrenaline to the brain. In the brain it is routed through areas that register the experience of this “fight/flight” chemical and send messages to the higher executive centers of the brain for interpretation.
It is in these cognitive areas of the frontal lobe that the messages of “attack” that came through autonomic nervous system are modulated and decisions are made about appropriate behavioral responses.
John no longer had the frontal lobe functioning, but the Inderal reduced the visceral internal organ responses of the autonomic nervous system. Since his peripheral nervous system’s ability to register stress - and thus to send “attack” messages - was reduced, John had fewer automatic behavioral responses. His recovery was limited by the extent of his injury, but he became calmer and more able to function appropriately.
Summary
The psychiatric disorder seen by the mental health clinician may be the first manifestation of the primary, physical or medical disease. With the dysregulation of normal brain functioning from the effects of trauma, damage, tumors, breakdowns in metabolism and degeneration, a depressive syndrome is often seen first in such primary diseases as Huntington’s chorea, multiple sclerosis, HIV, Parkinson’s, Cushing’s disease and systemic lupus erythematosus. Depression in the elderly might look like dementia and often is a precursor to dementia. (16)
It is difficult to differentiate symptoms in children from various medical conditions that present as depressive symptoms. For instance, anemia, brain injuries, chronic headaches, diabetes, drug abuse, epilepsy, infectious mononucleosis, hypothyroidism, Lyme disease, renal disease and Wilson’s disease (ex-foliative dermatitis) often present as depression. (16)
These medical illnesses are difficult to differentiate in the adult population where direct reporting is usual. Assessment among children and adolescents is even more difficult, as parents are often the only observers and reporters of symptoms or behaviors. Their reporting may be less than adequate due to minimization or denial. Other parents may be judged to be overprotective by mental health professionals and may not be taken seriously.
Care must be taken in all populations, since some of these are devastating illnesses. It is important that depression not be dismissed as normal in these cases because studies show that - whereas depression may be the first symptom in some cases -very few patients with these illnesses actually become depressed. (10) As we have stated earlier, a mental health professional may be the first person that clients encounter in their quest for relief, either through self-referral or through referral from primary care providers who suspect hypochondriasis.
Baseline laboratory studies should be considered to rule out organic components of the depressive symptoms, especially in children. Communication with a medical team is critical for treatment of the whole client/patient in all cases.
Summary Page
Depression/Anxiety Caused by or Indicating Medical Illness
WHAT THEY ARE:
Direct brain cell and tissue damage:
- Brain trauma
- Ischemia (cellular breakdown)
- Infarction (cerebrovascular accident-CVA-stroke)
- Abnormal neuron growth (tumor)
- Degenerative brain cell loss
Indirect brain cell and tissue damage:
- Dysfunctions of brain metabolism associated with diseases that poison the whole system
- Body trauma
HOW THEY CAUSE SYMPTOMS OF ANXIETY AND DEPRESSION:
Direct brain cell and tissue damage:
Brain trauma – blunt, penetrating or indirect:
- Direct damage kills brain tissue but also sends a shock wave through the brain causing tissue destruction distant from the initial trauma site
- Neurotransmitter pathways necessary for modulation of mood are interrupted
- Location of injury determines symptoms
Ischemia and Infarction:
- Lack of oxygen to the cells leads to a failure in ion exchange across cell membranes leading to ultimate cell destruction and severely altered neurotransmitter functioning
- Complete ischemia leads to stroke where depression is due to altered dopamine systems affecting mood and anxiety level
- Epinephrine required for learning and memory is affected
- Serotonin necessary for alertness, sense of well-being and information processing is compromised
Abnormal Neuron Growth/Tumor:
- Overproduction of mutated cancer cells take place of or hinder growth of normally functioning cells
- Neuronal transmission is impaired
- Proliferation of tumor cells compresses healthy brain tissue leading to ischemia
- Byproducts of cell metabolism lead to toxicity and destruction of brain tissue
Degenerative Brain Cell Loss
- Degenerative diseases can cause direct brain cell loss as they cause direct neuronal damage
- Changes can include loss of dopamine secretion and loss of dopamine receptor sites in transmitter pathways
- Decreased general functioning can lead to hopelessness and depression
Indirect brain cell and tissue damage:
Dysfunctions of Brain Metabolism Associated with Diseases and Disorders that Affect the Whole System:
- Any disease attacking the whole system can affect metabolism critical for brain activity, i.e. Multiple Sclerosis, Diabetes, Nutritional Disorders
- Delicate nutritional balance is critical for production of enzymes that keep the pathways functioning
- Diseases that affect the elimination of toxins or add high toxicity to the body further hamper normal cell development and functioning
Body Trauma:
- Can cause an imbalance in the body’s neurotransmitter response to threat
- Body systems increase norepinephrine with little buffer
- Cognitive and affective functioning is altered leading to symptoms similar to anxiety
- Where an imbalance persists there is destruction to physical body systems
CRITICAL ASPECTS OF ASSESSMENT:
Thorough assessment includes:
- Psychosocial history, including mental status exam and medication evaluation
- Physical/health history – diseases past and current, accidents, physical activities, nutrition, family history of illnesses, medications, pain issues, allergies, communication with primary care physician
- Factors affecting depression – location of lesion, family history, pre-morbid depression history, social functioning, degree of functional impairment
- Hidden or unusual causalities – direct trauma from soccer, whip lash, pain
- Special consideration must be taken with children as there may be under-diagnosis of medical conditions that often present as depression – anemia, brain injuries, chronic headaches, diabetes, drug use, epilepsy, infectious mononucleosis, hypothyroidism, Lyme disease, renal disease and exfoliative dermatitis
RISKS AND DANGERS IF LEFT UNTREATED:
Untreated medical illnesses can lead to continuous cellular destruction, more and more involvement of other body systems, temporary or permanent impairment of mental and physical functioning, and – ultimately – death
While this subject area is of tremendous importance for any clinician who wishes to provide a thorough assessment of a client's problems, it is outside the scope of this training. For clinicians who require further training in this area, it is recommended that yourceus.com's course on this topic be considered: DIFFERENTIAL DIAGNOSIS: IDENTIFYING COMMON MEDICAL CONDITIONS FREQUENTLY MISDIAGNOSED AS MENTAL HEALTH PROBLEMS.
Before moving to a discussion of the development of a clinical impression, there is one other area that warrant some examination: the use of measures in assessment.
